Gastric Bypass vs Gastric Sleeve: Which Weight Loss Surgery Better?
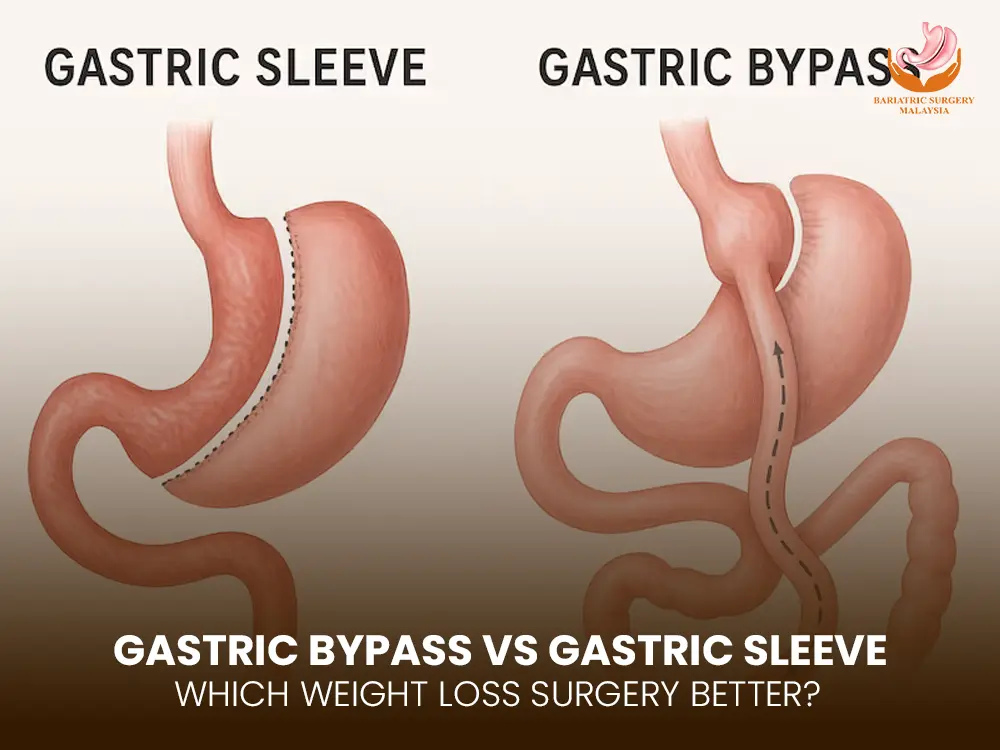
Gastric Bypass vs Gastric Sleeve: Which One Better? Obesity affects over 1.13 billion adults globally by 2030, up more than 115% from 2010, intensifying demand for effective bariatric interventions. (pmc.ncbi.nlm.nih.gov) In 2025, metabolic and bariatric surgery remains a gold standard — recent data shows these surgeries produce about 5× more weight loss over two years than GLP-1 drugs. (nyulangone.org) Between Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy (LSG), both have strong scientific backing, yet differ in mechanism, risk profile, nutritional demands, and long-term outcomes. This guide helps you compare both methods so you can decide which fits your health goals, comorbidities, and lifestyle best. How Each Procedure Works: Mechanism & Surgical Details Gastric Bypass (Roux-en-Y Gastric Bypass) Creates a small gastric pouch (~30 mL) and connects it to the small intestine, effectively bypassing a portion of the stomach and duodenum. Reduces food intake and nutrient absorption, leading to weight loss and favorable metabolic changes (hormone shifts, insulin sensitivity). It is a mixed restrictive and malabsorptive surgery. Gastric Sleeve (Sleeve Gastrectomy) About 75–80% of the stomach is removed, leaving a narrow “sleeve.” Primarily restrictive — limits how much you can eat, and also lowers the hunger hormone ghrelin, reducing appetite. No intestinal rerouting, so less malabsorption. Often preferred for patients who need significant weight loss but want fewer nutritional deficits. Indications & Eligibility Criteria Candidates are assessed via: BMI thresholds, obesity-related comorbidities, and failure of conservative therapies. Traditional criteria: BMI ≥ 40, or BMI ≥ 35 with conditions like type 2 diabetes, hypertension, obstructive sleep apnea. For Asian populations, the thresholds are often adjusted lower (e.g. BMI ≥ 32.5 or ≥ 27.5 with comorbidities). In 2025, bariatric procedures are also endorsed even for BMI 30+ in patients with metabolic disease. Other factors: age, surgical risk, gut anatomy, nutritional status, and willingness to adhere to lifelong follow-up. Calculate Your BMI Now and take the first step toward a healthier future. Expected Outcomes & Weight Loss Patterns Outcome Metric Gastric Bypass Gastric Sleeve % Excess Weight Loss (1–2 years) ~60–70% ~50–65% Diabetes remission rate High; often superior in long-term metabolic control Strong, especially in early disease Long-term durability Excellent when combined with adherence Very good, though some risk of weight regain Mechanism Restriction + malabsorption + hormonal changes Restriction + hormonal changes Studies show bariatric surgery still provides the most durable weight loss when combined with lifestyle changes compared to medical therapy alone. Advantages & Limitations: Pros vs Cons Advantages of Gastric Bypass Strong metabolic effect: better in diabetes remission and lipid control Greater weight loss in many severe obesity cases Potentially better long-term weight maintenance Limitations / Risks of Gastric Bypass More complex surgery, higher risk of complications Malabsorption of vitamins/minerals (iron, B12, calcium, fat-soluble vitamins) Risk of dumping syndrome Requires strict lifelong supplements Advantages of Gastric Sleeve Simpler technique, shorter operative time Lower risk of malabsorption Less nutritional deficiency burden Good weight loss for many patients with moderate to severe obesity Limitations / Risks of Gastric Sleeve Potential weight regain over time Staple-line leaks or bleeding Less metabolic effect in severe diabetes cases Not ideal if patient requires a malabsorptive component Surgical Risk & Complications Bariatric surgery has become safer over decades; major complication rates are around ~4%, and mortality is ~0.1%. Risk factors include surgeon experience, patient comorbidities, and procedure complexity. Potential complications: Anastomotic leak Bleeding Stricture / stenosis Nutritional deficiencies Internal hernia (especially after bypass) Marginal ulcers Gallstones or gallbladder disease Dumping syndrome (bypass) GERD exacerbation (sleeve) Choosing a high-volume, board-certified bariatric center is critical to reducing risks. Recovery & Follow-Up: What to Expect Most patients stay 1–3 days postoperatively (laparoscopic technique). Return to light activity in 1–2 weeks; full activity by 4–6 weeks. Diet progresses from liquid → pureed → soft → regular over 8–12 weeks. Lifelong vitamin and mineral supplementation (especially for bypass). Regular follow-up: nutritional labs (iron, B12, calcium, vitamin D), metabolic parameters, and behavioral support. Nutritional & Lifestyle Considerations Both surgeries require commitment to: High-protein, low-sugar diet Vitamin/mineral supplementation Behavioral therapy and lifestyle changes Frequent follow-up visits Bypass patients need stricter monitoring for malabsorption risks; sleeve patients may need surveillance for acid / reflux issues. Average Cost Gastric Bypass vs Gastric Sleeve In Malaysia (2025) Procedure Type Typical Cost (MYR) Notes / Sources Gastric Bypass RM 28,000 – RM 40,000 Private hospital packages listed by Bariatric Surgery Malaysia Gastric Sleeve RM 25,000 – RM 38,000 Listed among procedure-cost ranges for sleeve surgeries Notes & caveats: These costs usually include surgery, hospital stay, basic post-op care, and surgeon fees, but extra lab tests, nutrition counseling, extensions, or complications may add more. Public (government) hospital rates and subsidized pricing may be significantly lower. Location (Kuala Lumpur, Penang, etc.), surgeon expertise, hospital class, and technology used (robotic, minimally invasive) also strongly influence cost. Decision Factors: How to Choose What’s Best for You Consider the following in consultation with your bariatric surgeon: Severity of obesity / BMI / comorbidities Presence of type 2 diabetes or metabolic disease Willingness for strict nutrition and follow-up Risk tolerance / surgical fitness Preference for simpler procedure vs stronger metabolic effect Existing gastroesophageal reflux disease (GERD) – Bypass may help; sleeve may worsen Long-term goals and ability to maintain lifestyle changes Your surgeon should run imaging, nutritional labs, and anatomical evaluation to tailor the choice. Frequently Asked Questions (FAQs) 1. Which surgery leads to more weight loss long term?Gastric bypass often yields greater and more sustained weight loss, particularly in patients with severe obesity, but sleeve success is strong in many cases. 2. Is gastric bypass riskier than sleeve?Bypass has higher complexity and risk of complications and malabsorption. Sleeve is simpler, but still carries surgical risk. 3. Can type 2 diabetes go into remission?Yes. Bypass tends to have stronger remission rates, though sleeve also achieves remission in many patients, especially in early-stage disease. 4. What nutritional supplements are required?Bypass: multivitamin, iron, B12, calcium, vitamin D, often more. Sleeve: baseline supplements, possibly less aggressive monitoring of malabsorption. 5. Which surgery suits patients with
