Top 7 Benefits of Gastric Surgery: A Life-Changing Solution for Lasting Health

Gastric surgery, also known as bariatric surgery, has emerged as a transformative solution for individuals struggling with obesity. This procedure is not only about weight loss; it impacts overall health, lifestyle, and longevity. For those considering or researching this topic, this comprehensive guide explores the many benefits of gastric surgery, what to expect, types of procedures available, and essential tips for a successful recovery. What is Gastric Surgery? Gastric surgery refers to a group of surgical procedures designed to aid significant weight loss by making changes to the digestive system. This type of surgery is typically considered when diet and exercise have not yielded the desired results or when serious health problems related to obesity are present. The primary goal of gastric surgery is to limit the amount of food intake or decrease nutrient absorption, or sometimes both. Top Benefits of Gastric Surgery 1. Significant and Sustained Weight Loss One of the main reasons individuals opt for gastric surgery is the potential for substantial and lasting weight loss. Studies have shown that people undergoing these procedures often lose between 50-70% of their excess body weight within the first two years after surgery. This long-term weight loss can lead to improved mobility and a better quality of life. 2. Improvement or Resolution of Obesity-Related Conditions Gastric surgery can effectively manage or even resolve several health conditions associated with obesity, such as: Type 2 Diabetes: Many patients see a significant reduction in blood sugar levels, sometimes achieving complete remission. Hypertension: Weight loss helps in lowering blood pressure and reducing the risk of cardiovascular diseases. Sleep Apnea: The decrease in body weight contributes to a better night’s sleep and may eliminate the need for CPAP machines. 3. Enhanced Cardiovascular Health With decreased body mass comes a reduction in cardiovascular risk factors. Gastric surgery has been linked to lower blood pressure, improved cholesterol levels, and reduced risk of heart attacks and strokes. By achieving a healthier body weight, patients often experience better heart health overall. 4. Boost in Mental Health and Self-Esteem Obesity is often accompanied by feelings of depression, anxiety, and low self-esteem. Gastric surgery can improve emotional health by promoting weight loss, which, in turn, boosts self-confidence and overall mental well-being. 5. Increased Life Expectancy Studies indicate that individuals who undergo gastric surgery typically live longer than those who remain severely obese. The procedure significantly reduces the risk of premature death, especially from obesity-related diseases. 6. Improved Mobility and Physical Fitness Losing weight enables people to move more freely and engage in activities that were once too difficult. The increased energy levels after surgery encourage a more active lifestyle, promoting further weight loss and overall fitness. 7. Enhanced Quality of Life Patients often report better participation in social activities, higher work productivity, and overall life satisfaction. The reduced physical and psychological burden contributes to an enriched daily experience. Types of Gastric Surgery Understanding the different types of gastric surgery can help in making an informed decision. Below are the most common procedures: 1. Gastric Bypass Surgery (Roux-en-Y) This procedure involves creating a small pouch from the stomach and connecting it directly to the small intestine. This change reduces food intake and nutrient absorption, leading to significant weight loss. 2. Sleeve Gastrectomy During this surgery, about 80% of the stomach is removed, leaving a narrow tube-like structure. This smaller stomach limits the amount of food consumed and significantly reduces hunger by impacting hunger-regulating hormones. 3. Adjustable Gastric Banding A band is placed around the upper portion of the stomach, creating a small pouch that limits food intake. This method is less invasive, but the results may vary, and the band requires periodic adjustments. 4. Biliopancreatic Diversion with Duodenal Switch (BPD/DS) This complex procedure combines sleeve gastrectomy with an intestinal bypass. It’s highly effective for weight loss but comes with a higher risk of nutrient deficiencies and requires a strict post-surgery regimen. What to Expect Before and After Gastric Surgery Pre-Surgery Preparation Before undergoing gastric surgery, patients are usually required to meet specific medical and psychological criteria. This often includes consultations with a: Surgeon: To discuss the procedure, risks, and benefits. Dietitian: To plan pre- and post-surgery nutrition. Psychologist: To evaluate emotional readiness for the life changes that follow surgery. Patients might need to follow a special diet to reduce the size of the liver and facilitate a smoother surgery. Post-Surgery Recovery Recovery from gastric surgery involves several stages. Immediately after surgery, a liquid diet is typically recommended, gradually moving to pureed and soft foods before reintroducing solid foods. Patients must adhere to dietary guidelines to prevent complications and ensure lasting weight loss. Regular follow-ups with healthcare providers are crucial for monitoring progress and overall health. Tips for a Successful Gastric Surgery Journey Adopt a Healthy Diet: Eating nutrient-rich, portion-controlled meals supports weight loss and overall health. Stay Hydrated: Drinking enough water is essential for recovery and maintaining energy levels. Attend Support Groups: Connecting with others who have undergone gastric surgery can provide motivation and valuable advice. Commit to Regular Exercise: Physical activity accelerates weight loss and strengthens the body post-surgery. Adhere to Medical Advice: Follow-up appointments and vitamin supplementation are essential for avoiding deficiencies and complications. Potential Risks and Considerations While gastric surgery offers numerous benefits, it’s not without risks. Potential complications may include: Nutrient Deficiencies: Patients need to supplement vitamins and minerals due to limited food intake. Surgical Complications: These can range from infections to blood clots and should be discussed with the surgeon. Lifestyle Changes: Maintaining weight loss requires a commitment to a healthier lifestyle. Surgery is a tool, not a cure-all. FAQs About Gastric Surgery Is gastric surgery safe?Yes, gastric surgery is generally safe when performed by an experienced surgeon. However, as with any surgery, there are risks that should be discussed beforehand. How long is the recovery period after gastric surgery?The initial recovery period can last 3 to 6 weeks. Full recovery depends on the type of surgery and adherence to post-surgery
10 Transformative Facts About Operation to Lose Weight for a Healthier You

Weight loss can be challenging for many people, and standard diet and exercise might not always be enough. For those seeking significant and sustained weight loss, an operation to lose weight, known as bariatric surgery, could be the right solution. This article explores everything you need to know about these life-changing surgeries, helping you make an informed decision about your health journey. What Is an Operation to Lose Weight? An operation to lose weight, or bariatric surgery, involves medical procedures that aid in weight loss by altering the digestive system. These operations limit how much food a person can consume or how nutrients are absorbed. Common Types of Weight Loss Operations: Gastric Bypass: Reduces the stomach size and reroutes part of the digestive system. Gastric Sleeve Surgery: Removes a large part of the stomach, reducing its volume. Adjustable Gastric Band: Places a band around the upper part of the stomach to limit intake. Biliopancreatic Diversion with Duodenal Switch (BPD/DS): A less common but highly effective surgery that involves both restriction and malabsorption techniques. How Does Bariatric Surgery Work? Bariatric surgery changes the body’s metabolic functions. By reducing stomach size, patients feel fuller faster, leading to reduced food intake. Additionally, some surgeries change how the body absorbs nutrients, contributing to faster weight loss. Impact on Hormones: These procedures also influence the hormones that regulate hunger and satiety. The altered hormone levels can lead to decreased appetite and an increase in fullness after meals. Who Is Eligible for an Operation to Lose Weight? Bariatric surgery is not suitable for everyone. Specific criteria need to be met to qualify for an operation to lose weight: Body Mass Index (BMI): A BMI of 40 or higher, or between 35-39.9 with obesity-related health conditions like diabetes or high blood pressure. Previous Weight Loss Attempts: Candidates should have tried non-surgical methods, including diets, exercise, or medications, without achieving significant long-term results. Health Assessment: A comprehensive evaluation by a healthcare team to ensure the patient is fit for surgery. Benefits of an Operation to Lose Weight Bariatric surgery offers numerous benefits beyond significant weight loss. Here are the key advantages: 1. Improved Overall Health Many patients experience a dramatic reduction or even resolution of obesity-related conditions such as: Type 2 diabetes Sleep apnea Hypertension Joint pain 2. Enhanced Quality of Life Weight loss surgery can boost physical mobility, increase self-esteem, and enhance social interactions, contributing to a better overall quality of life. 3. Long-Term Weight Loss Success Studies show that many patients maintain long-term weight loss after an operation to lose weight, especially when combined with a healthy lifestyle. Risks and Considerations As with any surgical procedure, bariatric surgery comes with risks. Complications can include infections, blood clots, or nutritional deficiencies. To minimize risks, it is essential to choose a qualified bariatric surgeon and adhere to all pre- and post-surgical guidelines. Preparing for Bariatric Surgery Preparation for an operation to lose weight requires both mental and physical readiness. Here’s what to expect: 1. Medical Assessments A thorough medical evaluation to check for potential health risks and to create a tailored surgical plan. 2. Nutritional Counseling Nutritionists provide guidelines on pre-surgery and post-surgery diets. Patients are often advised to adopt a high-protein, low-carbohydrate diet to aid in recovery and maximize results. 3. Psychological Evaluation A psychological assessment ensures that patients are mentally prepared for the significant lifestyle changes ahead. Emotional support can be vital during the transition period post-surgery. Recovery After an Operation to Lose Weight Post-surgery recovery can vary by procedure but generally includes: Hospital Stay: Typically, a 1-3 day hospital stay is required. Diet Progression: Patients start with a liquid diet before moving to soft foods and eventually incorporating solid foods. Activity Levels: Light physical activity is encouraged soon after surgery to promote healing and prevent complications. Common Recovery Challenges: Adjusting to smaller meal sizes Monitoring nutrient intake to prevent deficiencies Ensuring adequate hydration Tips for Long-Term Success Post-surgery, lifestyle changes are crucial for maintaining weight loss. Here’s how to stay on track: Follow a Balanced Diet: A diet rich in lean proteins, vegetables, and whole grains is essential. Stay Active: Regular physical activity supports weight maintenance. Attend Follow-Up Appointments: Regular check-ups help track progress and manage any potential complications. Join Support Groups: Connecting with others who have undergone an operation to lose weight can provide motivation and encouragement. Cost of Bariatric Surgery The cost can vary widely based on location, type of surgery, and insurance coverage. In some cases, health insurance may cover the procedure if it is deemed medically necessary. FAQs About Operation to Lose Weight 1. How long does recovery take after weight loss surgery? Recovery time depends on the type of surgery, but most patients can return to normal activities within 4-6 weeks. 2. Will I need supplements after surgery? Yes, due to reduced food intake and potential nutrient malabsorption, most patients need to take daily vitamins and minerals. 3. Can the weight come back after surgery? Weight regain can happen if post-surgery guidelines are not followed. Maintaining a healthy diet and exercise regimen is crucial for long-term success. 4. What is the most effective bariatric surgery? The effectiveness varies per individual. Gastric bypass and BPD/DS are generally considered the most effective in terms of weight loss and health improvement. 5. Is bariatric surgery reversible? Some procedures, like the adjustable gastric band, are reversible. Others, such as gastric bypass, are generally permanent. 6. How soon will I see results? Most patients begin to see weight loss within the first few weeks post-surgery, with significant results within 6-12 months. Conclusion Weight loss surgery, also known as bariatric surgery, can be a life-changing intervention for individuals battling severe obesity. This surgical approach not only addresses physical health concerns such as diabetes, heart disease, and joint pain but also significantly impacts mental and emotional well-being. By reducing excess weight, individuals often experience improved self-esteem, increased energy levels, and a greater sense of overall life satisfaction. To achieve long-lasting
7 Life-Changing Insights About Stomach Operation for Bariatric Patients

A stomach operation, often part of bariatric surgery, has become a significant solution for people struggling with severe obesity. For many, this procedure can lead to profound health benefits, including substantial weight loss and improved quality of life. This article will explore key aspects of a stomach operation, detailing its types, benefits, risks, and what to expect during recovery. What is a Stomach Operation? A stomach operation refers to surgical procedures designed to help individuals lose weight by altering the stomach and sometimes the digestive tract. This type of surgery limits food intake, changes nutrient absorption, or both. It’s often recommended for individuals who have not achieved lasting weight loss through diet and exercise alone and have obesity-related health conditions. Types of Stomach Operations for Weight Loss There are several types of bariatric surgeries, each tailored to different needs and body types. Here’s an overview of the most common stomach operations: 1. Gastric Bypass (Roux-en-Y Gastric Bypass) One of the most widely performed bariatric surgeries, this operation involves creating a small pouch at the top of the stomach and connecting it directly to the small intestine. This bypasses most of the stomach and some of the small intestine. Benefits: Significant weight loss. Improvement in obesity-related conditions such as type 2 diabetes. Considerations: Permanent changes to the digestive system. Potential for nutrient deficiencies. 2. Sleeve Gastrectomy This operation involves removing a large portion of the stomach, leaving a tube-shaped section that holds less food. Pros: Simpler than gastric bypass with fewer complications. Reduced risk of nutrient deficiencies compared to gastric bypass. Cons: Irreversible. Some patients experience heartburn or acid reflux post-surgery. 3. Adjustable Gastric Band Also known as lap band surgery, this involves placing an inflatable band around the upper part of the stomach to create a smaller stomach pouch. The band can be adjusted or removed as needed. Advantages: Minimally invasive. Adjustable and reversible. Limitations: Slower weight loss compared to other procedures. Higher risk of needing follow-up surgeries to adjust or remove the band. Benefits of Undergoing a Stomach Operation Opting for a stomach operation can bring a range of physical and psychological benefits: Significant Weight Loss: Most patients experience substantial and sustained weight loss, improving their mobility and overall health. Reduction in Obesity-Related Conditions: Bariatric surgery has been shown to decrease or even resolve conditions like type 2 diabetes, sleep apnea, high blood pressure, and joint pain. Enhanced Quality of Life: With improved health and energy levels, many patients report higher self-esteem and a better overall quality of life. Risks and Potential Complications Like any surgery, a stomach operation comes with risks. It’s essential to weigh these against the benefits and discuss them thoroughly with your healthcare provider: Short-Term Risks: Infection at the surgical site. Blood clots. Adverse reactions to anesthesia. Long-Term Complications: Nutritional deficiencies, especially after bypass surgeries. Dumping syndrome, characterized by nausea, vomiting, or diarrhea when consuming high-sugar foods. Stomach pouch stretching or ulcers. Preparing for a Stomach Operation Preparation is key for a successful stomach operation and smooth recovery. Here’s what to keep in mind before surgery: 1. Pre-Surgery Assessments A comprehensive medical evaluation will be conducted to determine if you are a suitable candidate. Nutritional counseling is provided to help adjust your diet pre-surgery. 2. Lifestyle Adjustments Patients are usually advised to start a high-protein, low-calorie diet before surgery to shrink the liver and make the operation safer. Quitting smoking is essential as it can interfere with healing. The Recovery Process Post-Stomach Operation Recovery timelines and experiences vary depending on the type of stomach operation performed. Here’s what you can generally expect: Immediate Recovery: Hospital stays typically last 1-3 days, depending on the procedure. Pain management is provided, and patients are encouraged to move as soon as possible to reduce blood clot risks. Dietary Changes: A liquid diet is required initially, gradually transitioning to pureed and soft foods before returning to a regular diet. Hydration is crucial to prevent dehydration, as the smaller stomach can only hold limited amounts of liquid. Physical Activity: Light walking is encouraged within the first week of recovery. More intense physical activities can resume after approval from your healthcare provider, usually within 4-6 weeks. Psychological Impact and Support Undergoing a stomach operation can bring significant emotional and psychological changes. It’s not uncommon to experience feelings of euphoria from initial weight loss, followed by challenges related to body image and adapting to new eating habits. Support Groups: Joining a bariatric surgery support group can provide motivation, encouragement, and helpful tips from people who have undergone similar procedures. Therapy and Counseling: Consulting with a therapist specializing in weight loss or body image issues can be beneficial for long-term mental health. Long-Term Considerations A successful stomach operation requires commitment to a healthy lifestyle. Regular follow-up appointments are essential to monitor weight loss progress, address any complications, and ensure nutritional needs are met. Nutritional Supplements: Daily vitamins and minerals are typically needed to avoid deficiencies, especially after procedures like gastric bypass. Annual Check-Ups: These visits allow for early detection and management of potential complications, ensuring long-term success and health. FAQs About Stomach Operations Q1: Is a stomach operation reversible?Some types, like the adjustable gastric band, are reversible. Others, such as sleeve gastrectomy and gastric bypass, are permanent. Q2: How much weight can I expect to lose after a stomach operation?Patients typically lose 50-70% of their excess weight within the first year post-surgery, depending on the type of procedure and adherence to post-surgery guidelines. Q3: Will I have to follow a special diet for the rest of my life?Yes, maintaining a balanced diet rich in proteins, vitamins, and minerals is essential for sustained health and weight loss. Q4: How soon can I go back to work after the operation?Most patients can return to light work duties within 2-4 weeks, but this depends on the type of operation and the individual’s recovery. Q5: What lifestyle changes are necessary after surgery?Commitment to regular exercise, portion control, and avoiding high-sugar and high-fat foods is
Ultimate Guide to Lap Sleeve Gastrectomy: 7 Key Benefits and Considerations

Lap sleeve gastrectomy, often referred to as laparoscopic sleeve gastrectomy, is a popular bariatric surgery designed to aid in significant weight loss. This minimally invasive procedure involves the surgical removal of a portion of the stomach, creating a sleeve-like structure. As a result, the stomach’s capacity to hold food decreases, helping individuals manage their portion sizes and caloric intake effectively. In this article, we’ll explore the crucial benefits, the recovery process, potential risks, and considerations associated with lap sleeve gastrectomy to help you make an informed decision. What is Lap Sleeve Gastrectomy? Lap sleeve gastrectomy is a surgical procedure that reduces the stomach size by approximately 75-80%, leaving a banana-shaped “sleeve.” Unlike gastric bypass, this surgery doesn’t involve rerouting the intestines or altering nutrient absorption, making it a simpler, less invasive option for many individuals struggling with obesity. 7 Key Benefits of Lap Sleeve Gastrectomy 1. Significant Weight Loss Results One of the most compelling reasons patients opt for lap sleeve gastrectomy is its effectiveness in promoting weight loss. Most patients can expect to lose 50-70% of their excess body weight within the first year. The reduced stomach size restricts food intake, helping patients adapt to smaller, healthier meal portions. 2. Improved Metabolic Health The weight loss achieved through lap sleeve gastrectomy can lead to improved metabolic health. This includes the resolution or significant improvement of obesity-related conditions such as type 2 diabetes, hypertension, and sleep apnea. Many patients experience better blood sugar control and reduced dependency on medications post-surgery. 3. Minimal Invasiveness and Short Recovery Time Being a laparoscopic procedure, lap sleeve gastrectomy involves small incisions that reduce scarring and speed up the recovery process. Most patients can expect to return to light activities within 2-3 weeks and resume normal routines by 4-6 weeks, depending on their unique recovery pace. 4. Lower Risk of Nutrient Deficiency Compared to other bariatric surgeries like gastric bypass, lap sleeve gastrectomy has a lower risk of long-term nutrient deficiencies. While patients must adhere to a balanced diet and may need supplements, the risk of significant malabsorption is minimized because the intestines are left unaltered. 5. Reduced Hunger Hormone Production A lesser-known advantage of lap sleeve gastrectomy is its effect on ghrelin, the hunger hormone. By removing the part of the stomach responsible for producing ghrelin, many patients experience decreased hunger, making it easier to adhere to dietary changes post-surgery. 6. No Foreign Implants Unlike gastric banding, lap sleeve gastrectomy does not involve placing any foreign devices in the body. This reduces the risk of complications such as band slippage or erosion and eliminates the need for future adjustments or replacements. 7. Sustainable Lifestyle Change Lap sleeve gastrectomy isn’t just about rapid weight loss—it encourages long-term lifestyle changes. Patients often find that the smaller stomach size necessitates mindful eating habits and portion control, laying the foundation for sustained health benefits. Understanding the Risks and Considerations While lap sleeve gastrectomy has many benefits, it’s essential to understand the potential risks and considerations before proceeding. Surgical Risks All surgeries carry inherent risks. Common complications can include infection, bleeding, and adverse reactions to anesthesia. However, these risks are minimized when the procedure is performed by an experienced bariatric surgeon. Gastroesophageal Reflux Disease (GERD) Some patients may develop or experience worsened GERD after surgery. It’s crucial to discuss any pre-existing reflux issues with your doctor before considering lap sleeve gastrectomy. Weight Regain Potential While most patients achieve significant weight loss, maintaining that weight loss requires dedication to lifestyle changes, including a healthy diet and regular exercise. Without these, there is a risk of regaining weight over time. The Recovery Process: What to Expect After a lap sleeve gastrectomy, patients typically spend 1-2 days in the hospital for observation. The recovery process involves: Initial Post-Operative Phase: The first week after surgery focuses on liquid intake to prevent dehydration and allow the stomach to heal. Transition to Soft Foods: Around week 2-3, patients begin to incorporate pureed and soft foods. This gradual transition helps the stomach adapt. Return to Regular Diet: By 6-8 weeks, most patients can start eating regular, healthy foods, though in much smaller quantities than before surgery. Patients are advised to follow their surgeon’s guidelines closely to minimize complications and optimize recovery. Long-Term Outcomes and Lifestyle Adjustments Lap sleeve gastrectomy is only one part of a long-term weight management solution. Post-surgery, individuals must embrace a lifestyle centered around balanced nutrition, portion control, and physical activity. Consistent follow-ups with healthcare providers are also crucial to monitor progress and manage any nutritional deficiencies. FAQs about Lap Sleeve Gastrectomy 1. How long does a lap sleeve gastrectomy procedure take? The surgery typically takes 1-2 hours, depending on the patient’s specific situation and the surgeon’s expertise. 2. Is lap sleeve gastrectomy reversible? No, lap sleeve gastrectomy is not reversible as it involves the permanent removal of a portion of the stomach. 3. Can anyone undergo lap sleeve gastrectomy? Candidates usually have a BMI of 40 or above or a BMI of 35 or higher with related health issues like diabetes or hypertension. A thorough evaluation by a bariatric surgeon is necessary to determine eligibility. 4. What is the average weight loss after lap sleeve gastrectomy? Most patients lose about 50-70% of their excess body weight within the first 12-18 months after surgery. 5. Will I need to take supplements after the procedure? Yes, while the risk of severe nutrient deficiency is lower than with other surgeries, a multivitamin, calcium, and possibly other supplements are recommended to ensure nutritional health. 6. How soon can I return to work after the surgery? Most people can return to non-strenuous work within 2-3 weeks post-surgery, but this may vary depending on individual recovery. Conclusion Laparoscopic sleeve gastrectomy is a proven surgical intervention that offers significant benefits for individuals struggling with obesity and related health conditions. By restricting stomach capacity and altering hormonal signals, this procedure can lead to substantial and long-lasting weight loss. However, it’s important to note
Laparoscopic Sleeve Surgery: A Comprehensive Guide with Key Benefits and Considerations
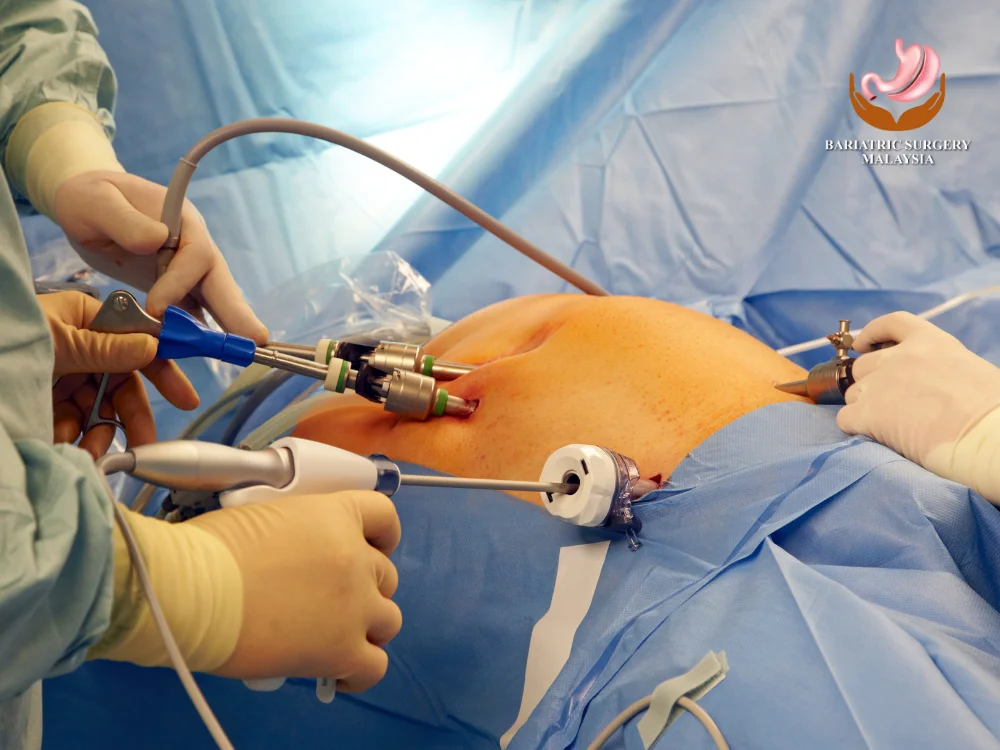
Laparoscopic sleeve surgery, known as sleeve gastrectomy, has surged in popularity as a leading weight-loss surgery. This minimally invasive procedure offers individuals significant weight reduction while ensuring a faster recovery and fewer complications compared to traditional open surgeries. Here’s an in-depth look at the key aspects of laparoscopic sleeve surgery, its advantages, potential drawbacks, and what patients can expect. What Is Laparoscopic Sleeve Surgery? Laparoscopic sleeve surgery is a type of bariatric surgery that reduces the stomach size to promote weight loss. The procedure involves making small incisions in the abdomen through which a laparoscope (a tiny camera) and surgical instruments are inserted. This method enables the surgeon to remove approximately 75-80% of the stomach, leaving a sleeve-shaped portion that limits food intake. How Does the Laparoscopic Approach Work? Unlike traditional surgery, the laparoscopic approach employs a minimally invasive technique: Small Incisions: The surgeon makes multiple small incisions rather than a large cut, which results in minimal scarring. Precision Tools: Specialized surgical instruments are used to carefully remove the excess stomach portion. High-Resolution Camera: A laparoscope provides a detailed view, ensuring precision during the procedure. Benefits of Laparoscopic Sleeve Surgery 1. Minimally Invasive Procedure Laparoscopic sleeve surgery is renowned for being less invasive than other forms of weight-loss surgeries. This leads to: Reduced Pain: Smaller incisions mean less pain post-surgery. Shorter Recovery Period: Patients can typically resume normal activities more quickly than with open surgery. 2. Significant and Sustained Weight Loss Patients who undergo laparoscopic sleeve surgery can expect significant weight loss, often losing up to 60-70% of their excess body weight within the first year. This weight reduction can greatly improve obesity-related conditions such as: Type 2 diabetes Hypertension Sleep apnea 3. Reduced Risk of Complications Since laparoscopic procedures are less invasive, there is a lower risk of complications like infections or hernias, which are more common with open surgery. Improved Quality of Life Weight loss following the surgery often results in: Enhanced physical mobility Better mental health Increased energy levels and participation in social and physical activities The Procedure: What to Expect 1. Preoperative Preparation Before undergoing a laparoscopic sleeve, patients typically go through: Comprehensive Evaluation: Health assessments and discussions with the surgeon to ensure candidacy. Dietary Guidelines: Pre-surgery dietary restrictions to optimize the body for surgery. Mental Health Support: Counseling may be suggested to prepare for lifestyle changes post-surgery. 2. Surgery Overview The surgery itself typically takes between one to two hours and follows these steps: The patient is placed under general anesthesia. The surgeon makes 4-5 small incisions in the abdomen. A laparoscope is inserted for real-time monitoring. The surgeon removes a significant portion of the stomach, creating the “sleeve.” The remaining portion is stapled shut. 3. Recovery and Aftercare Post-surgery, patients usually stay in the hospital for 1-2 days. Key aspects of recovery include: Pain Management: Mild pain managed with medication. Gradual Diet Progression: Starting with clear liquids and progressing to pureed foods before resuming solid meals. Lifestyle Adjustments: Incorporating a balanced diet and regular exercise is essential for long-term success. Potential Risks and Considerations While laparoscopic sleeve surgery boasts numerous benefits, it is not without risks. Common concerns include: Surgical Risks: Bleeding, infection, or reactions to anesthesia. Gastrointestinal Issues: Nausea, vomiting, or acid reflux may occur post-surgery. Nutritional Deficiencies: Due to reduced stomach capacity, nutrient absorption may be compromised, necessitating lifelong supplementation of vitamins and minerals. Comparing Laparoscopic Sleeve Surgery with Other Weight-Loss Surgeries 1. Laparoscopic Sleeve vs. Gastric Bypass Procedure Complexity: Gastric bypass involves rerouting the digestive tract, making it more complex than a sleeve gastrectomy. Nutrient Absorption: The risk of malnutrition is lower with laparoscopic sleeve surgery compared to gastric bypass. Weight Loss Rate: Both procedures offer significant weight loss, but gastric bypass may lead to slightly faster initial results. 2. Laparoscopic Sleeve vs. Adjustable Gastric Banding Surgical Invasiveness: Gastric banding is even less invasive but typically results in slower weight loss. Long-term Outcomes: Sleeve gastrectomy generally offers more consistent long-term weight maintenance. Lifestyle Changes for Post-Surgery Success Sustaining the benefits of a laparoscopic sleeve surgery requires significant lifestyle adjustments: Adopt Healthy Eating Habits: Small, nutrient-dense meals help manage the reduced stomach size. Regular Physical Activity: Integrating consistent exercise helps maintain weight loss and boosts overall health. Routine Medical Check-Ups: Regular follow-ups ensure that nutrient levels remain optimal and monitor for any potential complications. Frequently Asked Questions (FAQs) 1. Who is a good candidate for laparoscopic sleeve surgery? Candidates typically have a BMI over 40 or a BMI of 35-39.9 with associated health conditions. A thorough assessment with a bariatric specialist is essential for determining suitability. 2. How long is the recovery period after laparoscopic sleeve surgery? Most patients return to normal activities within 2-4 weeks, although full recovery can vary based on individual health factors. 3. Can weight be regained after surgery? Yes, while most patients maintain significant weight loss, poor lifestyle choices post-surgery can lead to weight regain. Commitment to a healthy lifestyle is key. 4. Are there dietary restrictions after the procedure? Yes, initial recovery involves a liquid and soft-food diet before gradually transitioning to solid foods. Long-term, balanced eating habits are recommended. 5. How soon after surgery can one resume exercise? Light activities can often be resumed within a week, while more strenuous exercise is typically recommended after 4-6 weeks. 6. Is laparoscopic sleeve surgery reversible? No, unlike gastric banding, sleeve gastrectomy is a permanent procedure. Laparoscopic sleeve surgery presents an effective path for individuals aiming for substantial, sustainable weight loss. By understanding the procedure, potential benefits, and the commitment required post-surgery, patients can make informed decisions that align with their health goals and lifestyles. View this post on Instagram A post shared by Bariatric Surgery Malaysia (@bariatricsurgerymalaysia)
