Endoscopy is a minimally invasive medical procedure that allows doctors to directly visualise the digestive tract using a flexible camera. It helps diagnose, monitor, and treat conditions such as ulcers, bleeding, inflammation, and cancer, often with same-day results, high accuracy, and a low risk of complications.
What Is Endoscopy?
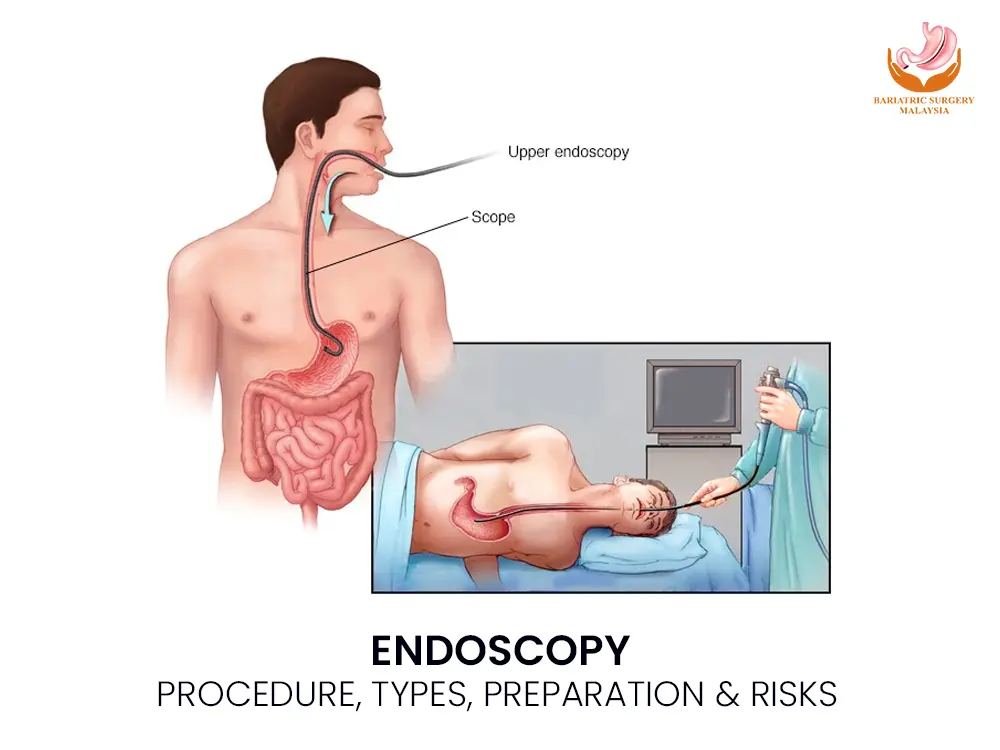
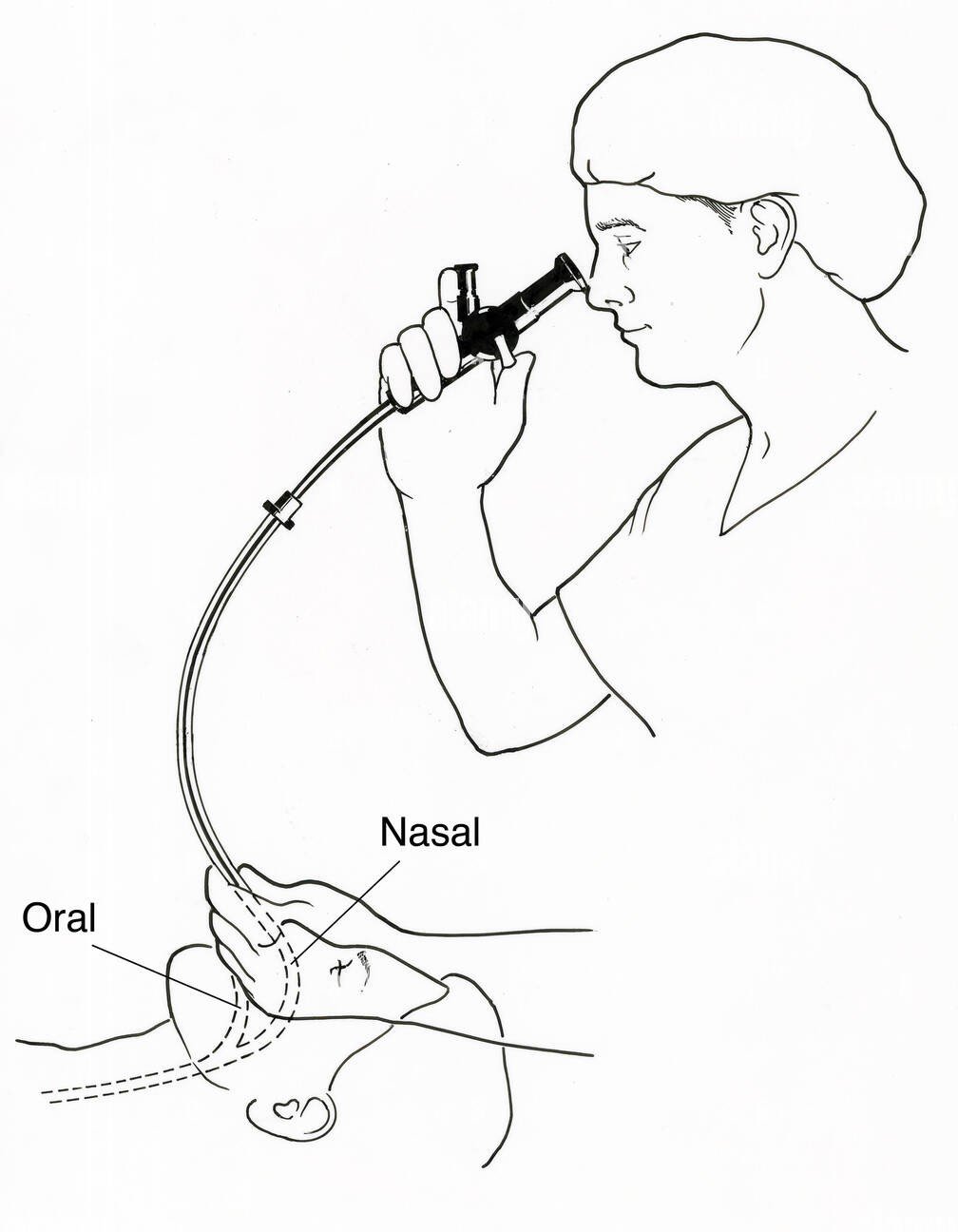
Endoscopy is a diagnostic and therapeutic procedure that uses a flexible endoscope—a thin tube equipped with a high-definition camera and light source—to examine the inside of the body. It is most commonly used to assess the upper and lower gastrointestinal tract, including the oesophagus, stomach, small intestine, colon, and rectum.
Unlike imaging tests, endoscopy allows direct visualisation of the mucosal lining, enabling doctors to detect subtle abnormalities, take biopsies, and perform treatment during the same procedure.
Types of Endoscopy Procedures
Upper Gastrointestinal Endoscopy (Gastroscopy)
Examines the oesophagus, stomach, and duodenum.
Common indications include:
Chronic acid reflux (GERD)
Gastritis and peptic ulcers
Helicobacter pylori infection
Upper gastrointestinal bleeding
Barrett’s oesophagus
Suspicion of upper GI cancer
Colonoscopy
Examines the entire colon and rectum, including the ascending, transverse, and descending colon.
Used for:
Colorectal cancer screening
Colon polyps and precancerous lesions
Chronic diarrhoea or constipation
Inflammatory bowel disease
Sigmoidoscopy
A shorter procedure focusing on the lower part of the colon.
Capsule Endoscopy
Uses a swallowable camera capsule to visualise the small intestine, especially when standard endoscopy cannot reach the area.
Endoscopic Ultrasound (EUS)
Combines endoscopy with ultrasound to evaluate deeper tissue layers, lymph nodes, pancreas, and nearby organs.
How Endoscopy Works (Mechanism of Action)
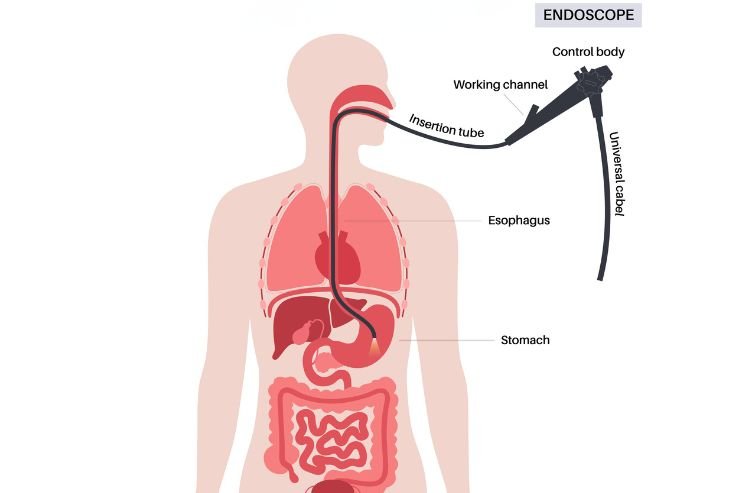
Real-time imaging via fibre-optic or digital chip technology
Light transmission illuminates internal structures
Carbon dioxide or air is gently insufflated to expand the organ
Abnormal tissue is identified visually
Biopsy forceps allow painless tissue sampling
Therapeutic channels enable treatment during the procedure
This direct approach makes endoscopy more accurate than scans for many digestive conditions.
Why Is Endoscopy Done?
Diagnostic Purposes
Persistent abdominal pain
Difficulty swallowing
Unexplained weight loss
Gastrointestinal bleeding
Anaemia of unknown cause
Chronic bowel habit changes
Therapeutic Uses
Removal of polyps (polypectomy)
Control of bleeding using clips or cautery
Dilatation of narrowed areas (strictures)
Removal of foreign objects
Targeted biopsies for cancer diagnosis
Conditions Diagnosed or Treated with Endoscopy
Gastritis and erosions
Peptic ulcer disease
Gastroesophageal reflux disease (GERD)
Varices
Strictures
Dysplasia and precancerous lesions
Inflammatory bowel disease
Gastrointestinal cancers
Early detection through endoscopy significantly improves treatment outcomes.
Preparation Before Endoscopy
Preparation depends on the procedure type:
Fasting for 6–8 hours (gastroscopy)
Bowel cleansing agents (polyethylene glycol solutions) for colonoscopy
Review of medications, especially blood thinners
Disclosure of allergies, pregnancy, or chronic medical conditions
Proper preparation ensures clear visibility and accurate results.
Sedation and Medications Used
Most procedures use conscious sedation, allowing comfort while maintaining breathing reflexes.
Common agents include:
Local anaesthetic throat spray (lidocaine)
Intravenous sedatives (midazolam)
Analgesics (fentanyl)
Vital signs are continuously monitored throughout the procedure.
Is Endoscopy Painful?
Endoscopy is generally not painful. Patients may feel mild pressure or bloating due to air insufflation. Throat irritation or temporary drowsiness after sedation is common but short-lived.
Risks, Side Effects, and Safety
Endoscopy is considered very safe when performed by a board-certified gastroenterologist in an accredited medical facility.
Possible Risks (Rare)
Bleeding after biopsy or polyp removal
Gastrointestinal perforation (less than 1%)
Infection
Sedation-related breathing issues
Most patients recover fully within hours.
Aftercare and Recovery
Avoid driving or operating machinery for 24 hours if sedated
Resume light meals once swallowing is normal
Expect mild bloating or sore throat temporarily
Seek medical attention for severe pain, fever, vomiting, or bleeding
Biopsy results are usually available within 3–7 days
Who Should Consider Endoscopy?
Endoscopy is recommended for:
Adults over 45 with digestive symptoms
Individuals with a family history of gastrointestinal cancer
Patients with unexplained anaemia or bleeding
Those with abnormal imaging or blood test results
It is also a key tool for cancer screening and prevention.
Frequently Asked Questions (FAQ)
Is endoscopy used for cancer screening?
Yes. It detects early cancer and precancerous changes, especially in the stomach and colon.
Will I be fully asleep during endoscopy?
Most patients receive conscious sedation, not general anaesthesia.
How accurate is endoscopy compared to CT scans?
Endoscopy is more accurate for detecting mucosal disease and allows biopsy.
How soon can I eat after endoscopy?
Usually within a few hours, once numbness wears off.
When will biopsy results be ready?
Typically within 3 to 7 days.
Can endoscopy treat conditions or only diagnose?
It can both diagnose and treat many conditions in the same session.
Conclusion: Prevention Saves Lives
Whether it’s managing IBD (Crohn’s or Colitis) or performing a routine cancer screening, endoscopy is a life-saving tool. It moves the conversation from “guessing” what’s wrong to “seeing” exactly what’s wrong. Finding a problem early—especially GI cancers—makes treatment much more successful.